Let’s talk about Prolapse…
Pelvic organ prolapse (also known as POP).
Let’s bust some myths and taboo’s surrounding prolapse.
Want to know, WHAT IS A PROLAPSE?
We need to take a look INSIDE our pelvis to answer this question. Within the pelvis, we have three organs: the bladder (which we pee out of), the uterus (where we have periods/babies grow) and the rectum (which we poo out of).
I love this hammock analogy.
The hammock represents your PELVIC FLOOR MUSCLES.
The yellow shape is your BLADDER organ.
The pink shape is your UTERUS organ.
The brown shape is your RECTUS organ.
One of the hammocks jobs is to keep the organs uplifted in the pelvis. It is a dynamic structure that is designed very well to adapt to the loads placed on it. It can stretch, support and tense. Think of your pelvic floor muscles like a trampoline; springy that can withstand heavy loads.
However, if the hammock gets damaged or becomes weak, it can lose its ability to support the pelvic organs and the strength to maintain its upright positions.
The pelvic organs may descend into the hammock via the vaginal walls as a result.
An anterior prolapse or cystocele is when the BLADDER descends into the FRONT wall of the vagina.
A posterior prolapse or rectocele is when the RECTUM descends into the BACK wall of the vagina.
A Uterine prolapse is when the UTERUS descends into the VAGINAL CANAL apically (from the top).

Learn about…
Prolapse – what, where, why
What are the signs and symptoms to look out for and how to manage them
Where to get help
Stages of prolapse
Prolapse treatment suggestions
Prolapse and periods
Prolapse and sexual function
A boat in a dry dock
I love a good visual and here is one that we are taught as physiotherapist’s to help explain pelvic organ prolapse to patients.
The boat in the dry dock analogy was created by Prof. Peggy Norton who first suggested pelvic organ prolapse is due to more than one structure in the pelvis.
The boat = pelvic organs,
The water = the pelvic floor muscles,
The cables = pelvis ligaments.
The arrows = external forces (Eg. cough, laugh, lifting heavy weights).
In optimal function, all these structure work in harmony and the boat floats nicely on the water in the dock.
When there is damage or a weakness to the pelvic floor muscles, the water depletes and leaves the cables taking all the strain to support the weight of the boat. Eventually, the boat sinks down into the dock just like your pelvic organs do with prolapse.
Hence prolapse is known as “the boat in a dry dock”. This visual helps people to understand their pelvis mechanics better and can help with their perception of prolapse.


Prolapse Stats
1:3 ladies who have had one or more children WILL develop PROLAPSE. That is a staggering amount! That’s people in their 20’s after their first pregnancy, or people who hit menopause and their obstetric history catches up with them.
It’s not just old ladies that prolapse happens to.
IT ALSO AFFECTS WOMEN WHO HAVE NOT HAD ANY CHILDREN! Especially if they lift heavy weights, are overweight or smoke or suffer with a chronic cough.
So, prolapse is COMMON, but it’s NOT NORMAL and you don’t have to put up with it!
Knowledge is power. Prevention is key.
Treatment is available and help is at hand with pelvic health physiotherapists – take a look at How to find a physio near you
How do I know if I have a prolapse?
Could you have a prolapse?
The common signs and symptoms may include a sensation of “heaviness”, “dragging down”, “hanging down”, “bulging”, “bulky” feelings in your lower pelvis/vaginal canal area or even your lower back region.
It may feel worse towards the end of the day.
Your bladder function may alter in one of the following ways:
- Slow flow when passing water
- Incomplete emptying
- Going to the toilet to wee more often (Frequency)
- Urgent desire to void your bladder (Urgency)
- Leakage when you cough, sneeze, laugh, jump (Incontinence).
Your bowel function may alter in one of the following ways:
- Constipation
- Incomplete emptying
- Needing to press the back of the vaginal wall to fully empty the bowel.
You might find when you insert a tampon for your period it falls out or won’t stay in properly.
A feeling of discomfort during sexual intercourse.
Prolapse is common, but it is not normal.

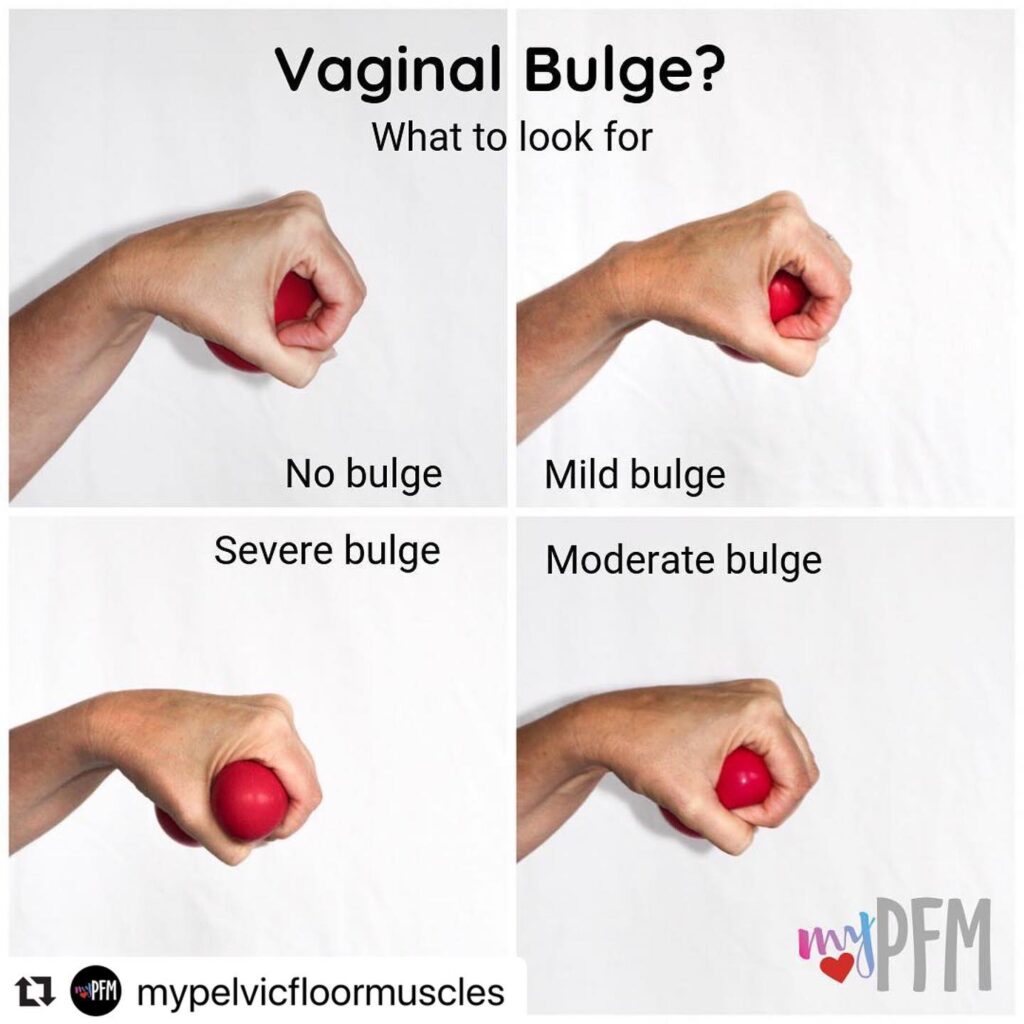
Not sure what to look for when checking for a bulge?
I’ve been asked a lot of questions about different stages of prolapse.
This visual is perfect again by the fabulous @mypelvicfloormuscles
- Mild bulge: generally difficult to see on self inspection
- Moderate bulge: a pinkish “ball” that does not go past the entrance of your vagina
- Severe: a pinkish “ball” that does go past the entrance of your vagina
Even though it may be the bladder or the rectum that is bulging, the bulge will be pinkish- it’s the colour of your vagina because what you are seeing IS your vagina.
Why is that?
How is a prolapse treated?
There are non-surgical and surgical options for the treatment of prolapse.
A prolapse can happen during pregnancy, just after childbirth or many years later and even to people who do not have pregnancies or give birth.
The majority of women (40%) have minor prolapses which have minimal or no symptoms.
Many people experience different symptoms with the same size of prolapse.
For some, it may affect their every move and for others, they may not notice it for the majority of time.
How ‘bothersome’ your prolapse symptoms are, normally defines your treatment.
Prolapse & Periods, lets talk about it…
It is not fully understood why you may feel your prolapse symptoms at certain times of your monthly cycle but here are a few theories;
⠀
1. Your uterus will change size during your menstrual cycle as the lining thickens after ovulation in preparation for a potential fertilised egg (or not) and then sheds it’s lining if no egg is fertilised or there like in an anovulatory period. (See period page for more info on this). It is likely before your period your uterus is heavier in bulk therefore prolapse symptoms may be felt more.
⠀
2. The pelvic organs are dynamic structures that change in their size according to when they are full or empty (think full bladder, needing to poo, or when you are on your period). They are not held in rigid positions inside our pelvis which could contribute to bothersome symptoms.⠀
3. During your menstrual cycle huge hormonal changes occur which are likely to alter your symptoms.
⠀
Sex and prolapse, are you worried about this?
This topic is very rarely talked about so let’s bust some myths!
Will having sex make my prolapse worse?
In one word, no.
It is safe to have sex and it will not damage your bladder/uterus or bowel. You may need to experiment with different positions or use a lubricant to make things more comfortable. The main message is it’s ok to try new things out. If you have pain though do discuss this with your GP to find out about other treatment options.
Will my partner feel my prolapse?
In a word, no.


Pelvic floor exercises with a prolapse: a great position to start with…and then progress to upright!
Start lying down with your hips elevated on cushions = GRAVITY ASSISTED.
Ly down flat on your back = GRAVITY NEUTRAL
Go into a semi plough position = GRAVITY ASSISTED BALANCING
I would add SITTING in here as the in between phase from lying to standing position.
Stand upright = ANTI-GRAVITY
Squat position = ANTI-GRAVITY SQUATTING
Jump = ANTI-GRAVITY JUMPING
As you can see there are a variety of positions you can use to help challenge or rest your pelvic organs in.
Related blog posts to prolapse…
Prolapse & Periods, lets talk about it…
Prolapse & Periods, lets talk about it... It is not fully understood why you may feel your prolapse symptoms at certain times of your monthly cycle but here are a few theories; ⠀ 1. Your uterus will change size during your menstrual cycle as the lining thickens...
How is pelvic organ prolapse treated?
How is pelvic organ prolapse treated? There are non-surgical and surgical options for the treatment of prolapse. A prolapse can happen during pregnancy, just after childbirth or many years later and even to people who do not have pregnancies or give birth. The...
What are the stages of prolapse?
What are the stages of prolapse? If you're not sure what to look for when checking for a bulge, read on. I’ve been asked a lot of questions about different stages of prolapse. This visual is perfect again by the fabulous @mypelvicfloormuscles Mild bulge: generally...
Resources
Instagram accounts to follow:
@popuplift | @mypelvicfloormuscles | @clarebournephysio | @hypopressiveguru | @pelvicroar | @adoreyourpelvicfloor | @gussetgrippers | @physiomumuk
POGP
Pelvic Organ Prolapse – A physiotherapist guide for women
Fit for Surgery: A physiotherapist guide
Please visit my Pelvic Health page for more useful resources



